The distinctive sound of tuberculosis heard through a stethoscope, often described as firecrackers, can be unsettling. This auditory clue, coupled with diagnostic tools used by the World Health Organization (WHO), aids in the early detection of this infectious disease. Pulmonologists specializing in respiratory illnesses, rely on auscultation to identify subtle sounds that signal potential issues. Understanding how tuberculosis up to the stethoscope the patient’s breathing sounds like firecrackers. is critical for healthcare professionals in regions facing high rates of tuberculosis, requiring careful evaluation to differentiate from other conditions.
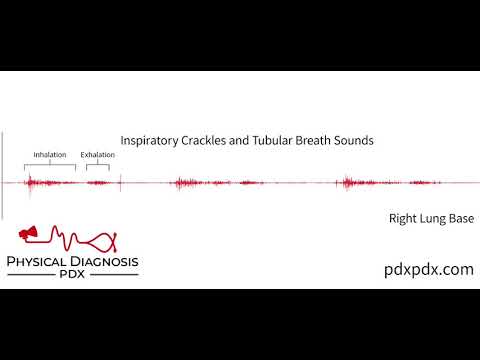
Image taken from the YouTube channel André Mansoor , from the video titled The Lung Sounds of Pneumonia .
The Curious Case of Firecracker Sounds in Your Lungs
Imagine listening to your breathing and hearing something unexpected—a crackling, popping sound, almost like tiny firecrackers going off inside your chest.
It’s unsettling, right?
This peculiar auditory phenomenon, detectable with a stethoscope, can sometimes indicate a serious underlying condition, and it’s a sound that medical professionals take very seriously.
One potential culprit behind these "firecracker" sounds is Tuberculosis (TB), a respiratory infection that continues to impact global health.
But what exactly causes this unusual lung sound, and why is it so important?
Unveiling the Mystery of Lung Sounds
When a healthcare provider uses a stethoscope to listen to your lungs, they’re listening for more than just the regular rhythm of breathing.
They’re searching for any abnormal sounds that might indicate a problem.
Crackles, also known as rales, are one such abnormality.
In the context of TB, their presence can be a crucial clue.
Tuberculosis (TB) is an infectious disease caused by the bacterium Mycobacterium tuberculosis. It primarily affects the lungs, but can also impact other parts of the body.
When TB damages the lung tissue, it can create an environment where fluids accumulate in the tiny air sacs called alveoli.
This fluid buildup is often the source of the crackling, firecracker-like sounds.
Article Purpose
This article aims to unravel the mystery behind these unusual lung sounds, specifically those resembling firecrackers. We will delve into the connection between these sounds and Tuberculosis, exploring the mechanisms behind their generation, their diagnostic significance, and the necessary steps to take if you or someone you know experiences them.
Our goal is to provide clear, understandable information so that you can be better informed about your respiratory health and know when to seek medical attention.
Understanding Tuberculosis (TB): A Deep Dive
Tuberculosis (TB) remains a significant global health challenge, impacting millions worldwide. To truly understand the significance of the "firecracker" sound in the lungs, a comprehensive understanding of TB itself is essential.
But what exactly is Tuberculosis?
Simply put, it’s an infectious disease caused by the bacterium Mycobacterium tuberculosis. While TB most commonly affects the lungs (pulmonary TB), it can also spread to other parts of the body, including the kidneys, spine, and brain (extrapulmonary TB).
How Mycobacterium tuberculosis Affects the Body
The Mycobacterium tuberculosis bacteria are typically spread through the air when someone with active TB coughs, sneezes, speaks, or sings. When inhaled by a new host, the bacteria can travel to the lungs and begin to multiply.
The body’s immune system typically responds by attacking the bacteria, attempting to wall them off in structures called granulomas. These granulomas can prevent the infection from spreading, but they don’t always eliminate the bacteria entirely.
Impact on the Respiratory System and Lungs
When the immune system is unable to completely eradicate the Mycobacterium tuberculosis, the infection can cause significant damage to the lungs.
This damage can include the formation of cavities (holes) in the lung tissue, inflammation, and scarring. This destruction of lung tissue is what ultimately leads to the symptoms associated with active TB, and contributes to the creation of abnormal breath sounds such as crackles/rales.
Latent vs. Active Tuberculosis: A Critical Distinction
It’s crucial to understand the difference between latent TB infection (LTBI) and active TB disease.
-
Latent TB: In latent TB, the bacteria are present in the body, but the immune system is keeping them under control. The individual has no symptoms, is not contagious, and usually tests positive on a TB skin test or blood test. They don’t feel sick.
-
Active TB: In active TB, the bacteria are actively multiplying and causing disease. The individual experiences symptoms such as cough, fever, weight loss, and night sweats, and is contagious.
The transition from latent to active TB can occur if the immune system weakens, for example, due to HIV infection, malnutrition, or certain medications.
The World Health Organization’s Role in TB Eradication
The World Health Organization (WHO) plays a critical role in the global fight against TB. The WHO sets global targets for TB prevention, diagnosis, and treatment.
It also provides guidance and support to countries in implementing TB control programs. The WHO’s End TB Strategy aims to end the global TB epidemic by 2030, with ambitious targets for reducing TB incidence and mortality.
The WHO also emphasizes the importance of addressing the social determinants of TB, such as poverty and inequality, which contribute to the spread of the disease. Their continued efforts are vital in achieving a world free from TB.
Latent vs. Active Tuberculosis: A Critical Distinction
It’s crucial to understand the difference between latent TB infection (LTBI) and active TB disease. Someone with LTBI has TB bacteria in their body, but they are not sick because the bacteria are inactive. They don’t have symptoms, and they can’t spread the infection to others.
However, if the immune system weakens, the latent TB infection can progress to active TB disease. People with active TB disease are sick, have symptoms, and can spread the infection.
The World Health Organization (WHO) plays a pivotal role in the global fight against TB. They set international standards for TB care and prevention, conduct research, and provide technical assistance to countries battling the disease. The WHO’s efforts are critical in reducing the global burden of TB and moving towards its eventual eradication.
Crackles/Rales: Decoding the "Firecracker" Sound
The "firecracker" sound, technically referred to as crackles or rales, is an adventitious (abnormal) lung sound that can be a significant indicator of underlying lung pathology, particularly in the context of Tuberculosis. But what exactly are crackles, and why are they likened to the distinct popping of firecrackers?
Describing the Sound: A Symphony of Disrupted Airflow
Crackles are typically described as short, discontinuous, popping or bubbling sounds heard during inspiration (breathing in). The analogy to firecrackers is apt because the sounds are often sharp, brief, and can vary in intensity and frequency. Think of it as the miniature snap, crackle, and pop experienced on a warm summer evening.
These sounds aren’t musical like wheezes; rather, they are more akin to static or the rustling of cellophane. Their presence demands careful attention, particularly in patients with a known risk of TB.
The Mechanism: Fluid and Alveolar Dynamics
The underlying mechanism producing crackles involves the sudden opening of small air passages (alveoli) in the lungs that were previously collapsed or filled with fluid.
The alveoli are tiny air sacs where gas exchange occurs. When these sacs collapse due to fluid accumulation or inflammation, they stick together. As the person inhales, air forces these alveoli open, creating the characteristic popping or crackling sound.
Think of it like pulling apart two wet pieces of glass; the sticky resistance and the sound produced are similar to what happens within the lungs.
TB’s Destructive Impact: Setting the Stage for Crackles
Tuberculosis damages the lungs in several ways that can contribute to fluid buildup and alveolar collapse.
- Inflammation: The infection triggers inflammation in the lung tissue, leading to fluid leakage into the alveoli.
- Cavitation: In some cases, TB can cause the formation of cavities (holes) in the lungs, which can become filled with fluid or debris.
- Scarring: As the lungs heal from TB infection, scarring can occur. Scar tissue can reduce the elasticity of the lungs, making it more difficult for the alveoli to open and close properly.
All these factors create an environment conducive to the development of crackles. The presence of crackles in a patient with suspected or confirmed TB is a serious finding that warrants further investigation and appropriate treatment.
Distinguishing Crackles from Other Abnormal Breath Sounds
It’s vital to differentiate crackles from other abnormal breath sounds like wheezes, rhonchi, and pleural rubs. Each of these sounds points to a distinct underlying issue.
- Wheezes: These are high-pitched, whistling sounds typically caused by narrowed airways, often associated with asthma or bronchitis.
- Rhonchi: These are low-pitched, snoring-like sounds resulting from secretions or obstructions in the larger airways.
- Pleural rubs: These are grating or creaking sounds caused by inflammation of the pleura (the lining of the lungs), often described as similar to walking on fresh snow.
Unlike these continuous sounds, crackles are discontinuous and popping in nature. A skilled clinician can distinguish these sounds with a stethoscope, which is the first step toward accurate diagnosis and appropriate care.
The Stethoscope’s Role: Auscultation and TB Detection
Having explored the nature of crackles and their connection to TB, it’s time to examine the indispensable tool that allows medical professionals to detect these subtle, yet significant, sounds: the stethoscope.
The Art of Auscultation: Listening to the Lungs
Auscultation, the practice of listening to internal body sounds, is a cornerstone of physical examination. It offers a non-invasive way to assess the condition of the lungs and other organs. For respiratory health, auscultation provides vital clues, revealing abnormalities that might otherwise go unnoticed.
Medical professionals meticulously use the stethoscope to listen to breath sounds at various locations on the chest. They are trained to differentiate between normal vesicular sounds, bronchial sounds, and adventitious sounds like wheezes, rhonchi, and, of course, crackles.
The Stethoscope: A Window into the Respiratory System
The stethoscope amplifies these sounds, allowing clinicians to discern subtle changes in airflow and identify potential problems. The bell of the stethoscope is generally used for low-pitched sounds, while the diaphragm is better for higher-pitched ones. Careful placement and technique are essential for accurate interpretation.
By systematically listening to different areas of the lungs, doctors can map the distribution of these sounds. This helps pinpoint the location and extent of any underlying lung pathology.
TB Detection: The Stethoscope’s Critical Contribution
In the context of Tuberculosis, the stethoscope plays a crucial role in early detection and diagnosis. The presence of crackles, particularly in the upper lobes of the lungs, can be a red flag, suggesting potential TB infection. While crackles can be caused by other conditions, their presence warrants further investigation, especially in individuals at risk for TB.
Differentiating TB Crackles: A Matter of Experience
Experienced clinicians can often differentiate TB-related crackles from those caused by other conditions. TB crackles are often described as fine, late-inspiratory crackles, meaning they occur towards the end of inhalation. This distinction requires a keen ear and extensive clinical experience.
However, it’s important to remember that auscultation alone is not sufficient for a definitive diagnosis of TB. It serves as an important initial step, prompting further diagnostic tests. The stethoscope acts as a crucial first line of defense. It alerts medical professionals to the possibility of TB.
Having pinpointed how crackles, detected via stethoscope, can raise suspicion of TB, the question becomes: What happens next? How is a preliminary suspicion solidified into a definitive diagnosis, and what steps lead to recovery?
Diagnosis and Treatment: A Path to Recovery
While auscultation provides valuable initial clues, confirming a Tuberculosis diagnosis requires more definitive methods. The journey from suspecting TB to actively treating it is a carefully orchestrated process involving advanced imaging and laboratory analysis.
Beyond the Stethoscope: Confirming the Diagnosis
A chest X-ray is a crucial next step. It can reveal characteristic abnormalities in the lungs, such as cavities (holes) or infiltrates, which are suggestive of TB. However, X-rays aren’t always conclusive. Further tests are almost always needed to confirm a diagnosis.
The gold standard for TB diagnosis is the sputum test. This involves analyzing mucus coughed up from the lungs to identify the presence of Mycobacterium tuberculosis. Sputum samples are typically examined under a microscope (smear microscopy) and cultured to grow the bacteria, which takes several weeks. The culture allows for drug-susceptibility testing, which is vital for guiding treatment.
Newer, rapid molecular tests, such as nucleic acid amplification tests (NAATs), can detect TB DNA in sputum within hours, providing a much faster diagnosis and guiding treatment decisions. These tests are particularly useful in detecting drug-resistant strains of TB.
The Critical Importance of Early Diagnosis
Early diagnosis of TB is paramount, especially in cases of primary TB, the initial infection in someone not previously exposed. In children, primary TB can rapidly progress to severe forms of the disease, such as TB meningitis or miliary TB (widespread dissemination of the bacteria throughout the body). Early diagnosis and treatment can prevent these life-threatening complications.
Furthermore, early detection of TB is crucial for preventing transmission to others. Identifying and treating active cases helps to break the chain of infection within communities.
Treatment Options: A Multi-Drug Approach
Tuberculosis is a treatable disease, but treatment requires a prolonged course of multiple antibiotics. The standard treatment regimen for drug-susceptible TB typically involves a combination of four drugs – isoniazid, rifampin, pyrazinamide, and ethambutol – for the first two months, followed by isoniazid and rifampin for an additional four months.
Adherence to the full course of treatment is essential to completely eradicate the bacteria and prevent the development of drug resistance. Directly observed therapy (DOT), where a healthcare worker watches the patient take each dose of medication, is often used to ensure adherence, especially in high-risk populations.
Drug-resistant TB is a growing concern, requiring more complex and expensive treatment regimens with second-line drugs, which are often more toxic and less effective.
The Pulmonologist’s Role: Expert Management of TB
A pulmonologist, a doctor specializing in respiratory diseases, plays a central role in managing TB. They are experts in diagnosing and treating lung conditions and can provide comprehensive care for patients with TB.
Pulmonologists oversee the diagnostic process, interpret test results, develop individualized treatment plans, monitor patients for side effects of medication, and manage any complications that may arise. They also play a vital role in coordinating care with other healthcare professionals, such as infectious disease specialists and public health officials.
While sophisticated diagnostic tools are essential for confirming Tuberculosis, it’s crucial to remember that the first line of defense often lies with the individual. Being attuned to your body and recognizing potential warning signs is paramount in ensuring timely intervention.
Listen to Your Body: When to Seek Medical Attention
Your body is constantly communicating with you. Changes, especially those involving your respiratory system, should never be ignored.
Ignoring potential symptoms can have serious repercussions.
It’s a disservice to your health to dismiss persistent coughs or unexplained fatigue as mere inconveniences.
The Significance of Unusual Breath Sounds
Any deviation from your normal breathing pattern warrants investigation. The "firecracker" sound, medically known as crackles or rales, is a key indicator discussed earlier. However, recognizing it yourself without a stethoscope can be challenging.
Instead, pay attention to any wheezing, shortness of breath, or pain while breathing.
These symptoms, whether subtle or pronounced, should prompt a visit to your healthcare provider.
Beyond the Breath: Recognizing Other TB Symptoms
Tuberculosis isn’t solely defined by respiratory distress. The bacteria can affect various parts of the body, leading to a range of symptoms. While a persistent cough lasting three or more weeks is a hallmark sign, other indicators can be just as important.
These include:
-
Unexplained Weight Loss: A significant drop in weight without dietary changes.
-
Night Sweats: Drenching sweats occurring during sleep.
-
Fatigue: Persistent and overwhelming tiredness that doesn’t improve with rest.
-
Fever: A low-grade fever that lingers for an extended period.
-
Coughing up Blood or Sputum: This is a serious sign that requires immediate medical attention.
If you experience a combination of these symptoms, especially if you belong to a high-risk group (e.g., individuals with weakened immune systems, those who have been in contact with someone with TB, or people from regions with high TB prevalence), seeking medical attention becomes even more critical.
The Urgency of Prompt Action
Tuberculosis is a treatable disease, especially when diagnosed early. Delaying diagnosis and treatment can lead to severe complications, including:
-
Spread of Infection: TB can spread from the lungs to other parts of the body, such as the brain, spine, and kidneys.
-
Permanent Lung Damage: Untreated TB can cause irreversible damage to the lungs, leading to chronic respiratory problems.
-
Drug Resistance: Delayed or incomplete treatment can contribute to the development of drug-resistant TB, which is more difficult and costly to treat.
Remember, early detection saves lives. By listening to your body and seeking medical attention promptly, you empower yourself to take control of your health and embark on the path to recovery. Don’t hesitate to consult a healthcare professional if you have any concerns. Your well-being is worth it.
Tuberculosis Sounds Like Firecrackers? FAQs
Here are some frequently asked questions to help you better understand the unusual sound associated with tuberculosis.
What causes the "firecracker" sound in tuberculosis patients?
The crackling, popping sound, where tuberculosis up to the stethoscope the patient’s breathing sounds like firecrackers, often indicates the presence of fluid or inflammation in the small air sacs (alveoli) of the lungs. This is due to the inflammatory response triggered by the tuberculosis bacteria.
Is the "firecracker" sound always present in tuberculosis cases?
No, the "firecracker" sound, where tuberculosis up to the stethoscope the patient’s breathing sounds like firecrackers, is not always present. It depends on the severity and location of the infection within the lungs, and whether there’s fluid or inflammation in the alveoli. Other symptoms might be more prominent.
Does hearing the "firecracker" sound immediately confirm a tuberculosis diagnosis?
No, while the sound, where tuberculosis up to the stethoscope the patient’s breathing sounds like firecrackers, can be a clue, it’s not conclusive. Other lung conditions can also cause similar sounds. Diagnostic tests like sputum cultures and chest X-rays are needed to confirm a TB diagnosis.
What other symptoms should I look for besides the "firecracker" sound?
Common TB symptoms include persistent cough (sometimes producing blood), fever, night sweats, weight loss, fatigue, and chest pain. If you experience these symptoms, especially if the patient’s breathing sounds like firecrackers due to tuberculosis up to the stethoscope, consult a healthcare professional for evaluation and testing.
So, next time you hear about tuberculosis up to the stethoscope the patient’s breathing sounds like firecrackers., remember it’s a key sign doctors listen for! Hope this cleared things up a bit – stay healthy!